Impact in MSK Physiotherapy – Part 1: Micro

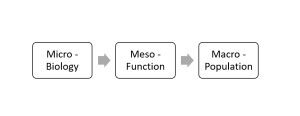
This first of our three-part series describes what MSK physiotherapy can actually do to biology via its perceived interventions. The meso will then extend this to function, while macro views MSK physiotherapy within a population-based approach.
Historically, MSK physiotherapy offered strengthening, stretching, exercise-based models, coupled with adjuncts such as manual techniques, electrotherapy and taping, plus many others.
The belief was to ‘alter’ the tissues/ biologically to a more advantageous state, enabling recovery and return to normal with reductions in pain.
It became clearer that interventions cannot be easily measured, and linked directly to cause and what we believed we were doing was very unlikely to be the case.
Let’s look at some examples of perceptions and counter views:
Stretching for example may not change the mechanical properties but could change the individual’s tolerance to an end of range discomfort, so this is really a pain tolerance change rather than tissue (Muanjai et al 2017).
When it comes to helping pain or discomfort in the workplace, stretching could be helpful (Gasibat et al 2017) but we do not know why that might be. Stretching protocols essentially might just be adaptive at a more sensory experience level than tissue based as very little change is seen in terms of architecture or tissue properties (Freitas et al 2018).
When as clinicians we look to strengthen the tissue in response to load and life, what might be happening?
There are so many trials or systematic reviews that offer different perspectives (Kooiker et al 2014; Powell and Lewis 2021), the list is endless, but once again there is no formula here and no correlation between the amount of strength gained, the pain reduction or the function improved.
Far more complex than what we were led to believe. Perhaps the belief in the process, the feeling of confidence, or the positive process of taking control through load-based exercises, could be just as powerful, if not more, than fibre type change that then leads to the change in experience (Skou et al 2014).
Psychological distress and sleep are intertwined with confidence, strength and pain (Fábrega-Cuadros et al 2020), so then we cannot assume anything other than inter-dependence, and that building those constructs into any programme is likely to be helpful, rather than strengthening alone.
Tissue changes in manual therapy as a concept seems pretty flawed, and certainly anything experienced would be a temporary experience. Perhaps tone of muscles might see alteration, but this is inconsistent and not maintained, pain experience alters but this is multi-factorial and cannot really be attributed a “force” or “procedure” (Dishman & Burke 2003; Pickar 2002).
However, patients can “feel better” for experiencing “treatment”, and can improve with specific exercise and benefit from movement, but perhaps this is only constructed within a clinical reasoned framework that from 30 years ago was simplified such as:
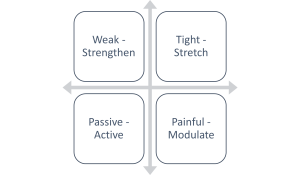
And perhaps things became over-complicated with over-searching for tissue causes (if we consider the SIJ or Core stability as good examples) whilst missing contextual effects, which have now perhaps moved the micro and its reasoning back to the basics above.
We now might consider those still, but look towards how they impact function and lifestyle rather than measuring a contraction, viewing a dial or seeing a number on a screen?
Therefore, building the micro and stopping there limits any outcome or potential, and so how MSK physiotherapy then lends itself to function and life seemingly should be the natural link, which perhaps was lost in those earlier explorations into the “effects” of therapy.
We will offer a short piece on this next week.
References
Dishman, J.D. and Burke, J., 2003. Spinal reflex excitability changes after cervical and lumbar spinal manipulation: a comparative study. The spine journal, 3(3), pp.204-212.
Fábrega-Cuadros, R., Aibar-Almazán, A., Martínez-Amat, A. and Hita-Contreras, F., 2020. Impact of psychological distress and sleep quality on balance confidence, muscle strength, and functional balance in community-dwelling middle-aged and older people. Journal of clinical medicine, 9(9), p.3059.
Freitas, S.R., Mendes, B., Le Sant, G., Andrade, R.J., Nordez, A. and Milanovic, Z., 2018. Can chronic stretching change the muscle‐tendon mechanical properties? A review. Scandinavian journal of medicine & science in sports, 28(3), pp.794-806.
Gasibat, Q., Simbak, N.B., Aziz, A.A., Petridis, L. and Tróznai, Z., 2017. Stretching exercises to prevent work-related musculoskeletal disorders: A review article. AJSSM, 5(2), pp.27-37.
Kooiker, L., Van De Port, I.G., Weir, A. and Moen, M.H., 2014. Effects of physical therapist– guided quadriceps-strengthening exercises for the treatment of patellofemoral pain syndrome: a systematic review. journal of orthopaedic & sports physical therapy, 44(6), pp.391-402.
Powell, J.K. and Lewis, J.S., 2021. Rotator Cuff– Related Shoulder Pain: Is It Time to Reframe the Advice,“You Need to Strengthen Your Shoulder”?. Journal of Orthopaedic & Sports Physical Therapy, 51(4), pp.156-158.
Skou, S.T., Wrigley, T.V., Metcalf, B.R., Hinman, R.S. and Bennell, K.L., 2014. Association of knee confidence with pain, knee instability, muscle strength and dynamic varus–valgus joint motion in knee osteoarthritis. Arthritis care & research, 66(5), pp.695-701.