Developing students’ thinking around MSK rehab planning: The “So what, why and how” approach.

This Clinical Insight is a short reflection from a team member who has been asked to help first year physiotherapy students in how they can create management plans through the patient story and examination.
This process is reported by many students as a challenge, as they can get to the “nuts and bolts” of assessment and ask certain questions, but it is the challenge of what to do with that information that is the difficult next step.
Establishing ‘So What?’
In gaining some sense of how to translate clinical data into something meaningful the “So What, why and how” can be helpful.
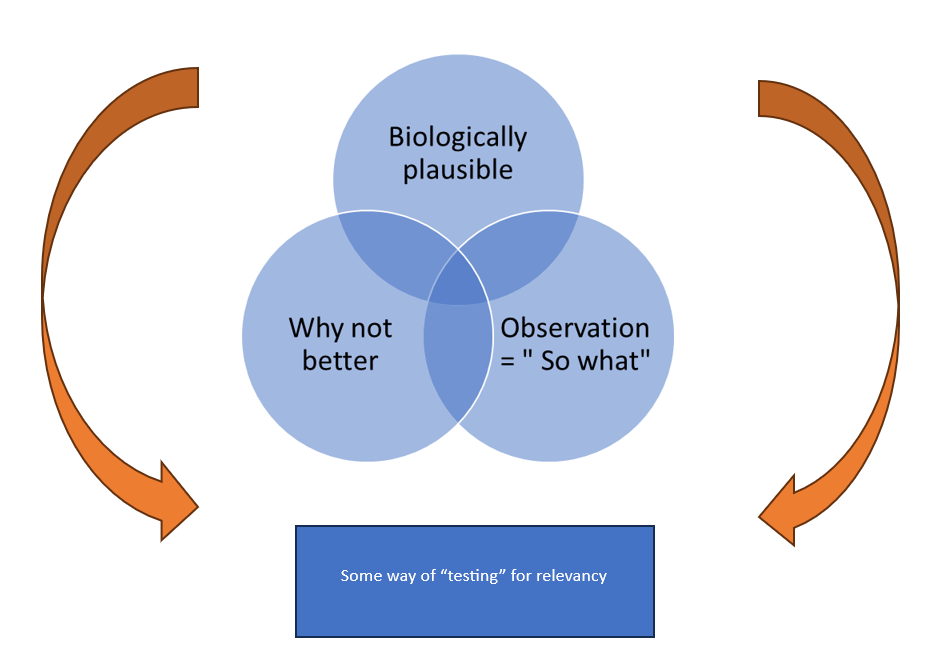
For example, the observation is a forward head posture, the question is then “so what?”, and that then lends itself to a deeper thought of relationship of findings to planning and the presentation. The linking of an observation into relevancy is one that is proposed to need clinical reasoning, but ultimately needs a number of different factors to just gain to a point of clinical legitimacy.
Let’s go back to the forward head posture. The “So What” might be that they have ongoing neck pain, (seems obvious) but this is a vital next step, as if we don’t apply this sensibly, everything is an observation.
We then apply “so what” again. So, the answer is they have not resolved their pain, and this COULD be a factor.
Linking the Why
We then have to link the why: “why not better?”. The patient has had a forward head posture for some time, so why pain now, what has changed? This could be their job, activity or stress levels. Something bothered the “status quo”, and it is this that is then building the “So What” answer.
They have a forward head posture, they have neck pain, it is not better naturally, something(s) are maintaining it. How will we know whether it is relevant? We need someway to give it further legitimacy.
How to Know if Relevant?
Let’s say we use palpation, with no more skill than, “is this bit sore?”. If we then modify the posture with simple advice, does this change how they feel in the same area. If not, this may be less useful (but not disregarded) but if yes, then this raises its relevance.
We place this in the proposed plan.
We note a stiff thoracic spine. Biologically plausible to be potentially part of the problem, but we can’t be more definite than that. So, what do we do?
Stiff thorax, So What? Well, a stiff thorax can mean muscles in the neck don’t gain quality movement. How will we know if this is potentially relevant? Try improving the thorax movement within the clinic or through a trial of exercise, to see if that works?
Sometimes we see something and it is irrelevant. A pronated foot with ongoing knee pain. The foot is unlikely to be a new feature, so once again, what’s stressed the system, why might it have changed? If we gain a simple test for pain and we can’t alter it with the foot position being changed it lessens the clinical relevancy.
Key Features of the “So what, why and how”
1. What’s changed? What prompted the change in experience.
2. Observations must be then thought of through “so what”.
3. Biological plausibility must be attached to the answer.
4. Some way of “testing” through examination and treatment are then employed.
To the experienced clinician, this is routine and of course part of practice, but if you have less experienced clinicians or students working with you, the “So what, why and how” is a great way to build the clinical plan, allow for deeper thought and create a framework to help build pattern recognition that is the vital component towards working with less cognitive challenge.
There are so many ways we might consider improving reasoning in students, and delivering simplicity from complexity is perhaps the key art of the practice educator?